Right knee medical history
This is part of an ongoing series of posts on what I have learned from an ongoing, chronic knee problem. This post describes how I injured my knee and has links to the posts I have written about other lessons I have learned.
This post is intended for orthopedic doctors and physical therapists.
Short version
This is as short a summary as I could make without losing any important information.
- ACL tear Jan 2019
- No pain after tear, did prehab exercises prior to surgery
- ACL reconstruction surgery (BTB patellar graft) Mar 2019
- Patellofemoral pain immediately after surgery that is present to this day
- Pain and stiffness are strongest in the last ~20º of extension
- Pain walking, particularly on flat terrain
- Started losing extension during rehab, found cyclops lesion, had it removed Dec 2019
- Constant, disciplined PT 2019-2022.
- Tried managing my pain as patellofemoral pain. Tried to keep pain 3/10 or lower and slowly built up strength, i.e. envelope of function approach.
- Never able to restore normal function
- Tried returning to agility/running but always ended up encountering large spikes in pain, and the movement never felt normal
- Tried “knee-safe” activities like swimming, but the kicking was very painful for me
- Kaiser surgeons told me that long-term, unresolvable patellofemoral pain is possible with any ACL surgery, and more likely with my graft choice.
- In my surgeries and MRIs, Kaiser PTs and surgeons noted cartilage wear behind my patella, suggested that was the cause of pain
- I became disillusioned with Kaiser, switched to Anthem to gain access to a broader set of doctors and institutions
- Several surgeons point out the cartilage wear in my MRIs and suggested patellar MACI
- MACI harvest Aug 2022, implantation Sep 2023
- Was quickly evident that MACI had no impact on my pain, experienced same pain and stiffness as I have since initial ACL surgery
- Post-MACI PT, following envelope of function approach again
- Unfortunately, pain levels continue to increase
- Paid out-of-pocket for an MRI of my good knee
- Learned that I have the same cartilage wear in the same location on my good knee, which does not present with any pain
- Pain near extension worsened 2024-2025 to the point where even walking can be very painful
- Currently only able to cycle with a manageable amount of pain. Squats, hiking, swimming, even walking are all painful. Jogging and running are inconceivable.
- Renewed search for an orthopedic doctor who could help me figure out what is going on, new x-ray and MRI performed
- Details below
All MRI reports and post-op notes
All my MRI reports and post-op notes are available here.
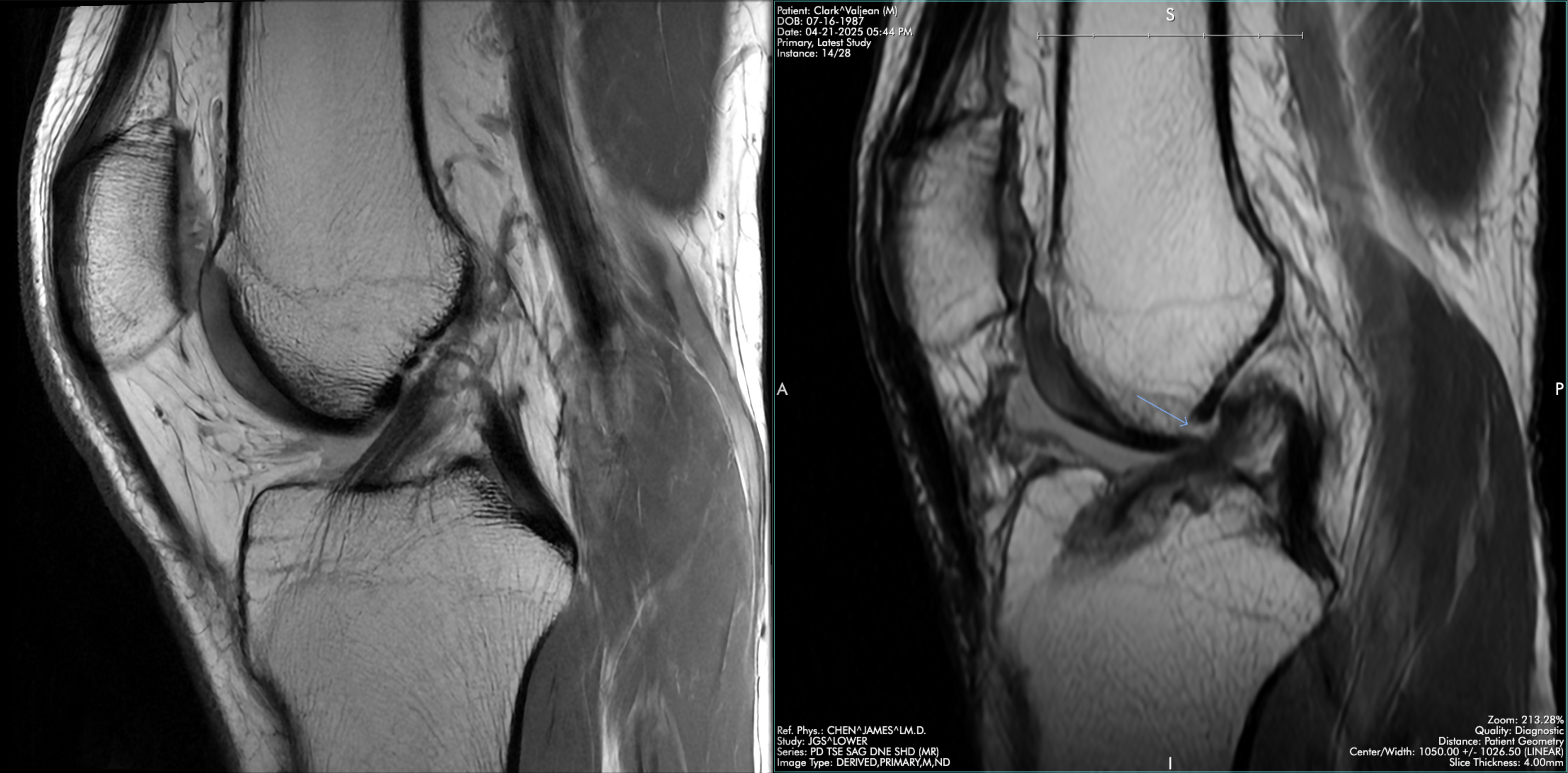
The image below shows a side-by-side MRI comparison of my good knee’s ACL and my right knee’s ACL. The anterior placement of the graft, bowing, and impingement are all visible.
Full version
I tore my ACL skiing in January 2019. ACL reconstruction surgery was soon scheduled for March 2019 at Kaiser in San Francisco. For the 2 months before the surgery, I did “prehab” to keep the knee and leg strong. I was pain free at this time.
I was given a choice between a hamstring graft and a BTB patellar graft. The surgeon advised me to do the BTB patellar graft because it is the “gold standard” and the graft is stronger than the hamstring graft, and hence more resistant to re-tear.
As soon as I started PT exercises after my ACLR surgery, I started experiencing pain and stiffness that has stayed with me to this day. The pain presents under and slightly below my patella, and it is strongest in the ~20º arc leading up to full knee extension. Consequently, it is easy to trigger with simple PT exercises like quad sets and banded terminal knee extensions. Kaiser PTs encouraged me to “push through the pain”, but it was clear my experience was different than the others in my group PT sessions. The pain was blocking me from being able to perform movements correctly.
After initially regaining extension, I started to lose extension a few months into PT. Because of this and the strong patellofemoral pain I was experiencing, while my rehab stalled. After another MRI, we discovered that a cyclops lesion had developed. Another surgery was performed in December 2019, after which I regained extension. The hope was that this, combined with some debridement, would reduce pain, but it did not.
I spoke with several different surgeons at Kaiser about my situation, and they all said 1) that BTB patellar graft can result in unresolvable patellofemoral pain and 2) given my cartilage damage, I could consider a cartilage restoration surgery like OATS.
Disappointed with the quality of Kaiser’s PT department and skeptical that more surgery would fix my problems, I left Kaiser to gain access to a broader set of institutions, PTs, and doctors. I found some PTs who treated my condition as they would general patellofemoral pain, which allowed me to restore some strength and function. This envelope of function approach instructed me to keep pain 3/10 or below and slowly build up strength while avoiding any movements that cause spikes in pain. This allowed me to regain a lot of muscle mass, and it also made it possible to return to hiking and cycling. These activities were still not pain free, but I could do them at a seemingly manageable low level of pain.
I tried reintroducing running at multiple points, but it would always lead to large spikes in pain that took weeks to recover from. Over time, my pain levels kept increasing with activities like hiking and weightlifting. I had an MRI done and found that the cartilage damage to my patella had expanded to become a 2cm defect. I had several different surgeons look at this MRI (Brian Gilmer, Drew Lansdown, and Ken Akizuki), and all 3 mentioned MACI as an alternative to OATS for cartilage restoration.
With pain worsening, I decided I needed to try another surgery, and it seemed like I had consensus that MACI was worth a try. (Aside: I learned recently that not all surgeons are as optimistic about MACI’s effectiveness, particularly for a large patellar defect, so it seems I just had a sample of surgeons biased toward MACI.) I had the MACI graft implanted in Sep 2023.
A few months into the PT for MACI, it became clear that it did not have any impact on the pain. All the same exercises involving terminal knee extension still hurt. Walking on flat surfaces still hurt. Discouraged but still determined, I spent the following year rehabbing using the same envelope of function approach as before.
Given all the focus on cartilage, my PT suggested that I could pay out-of-pocket for an MRI of my good knee to get a better idea of the state of the cartilage in my good knee as a baseline. This ended up being very interesting - the MRI showed that I have similar cartilage damage in the same area on my good knee. Between the MACI and this MRI, I became quite skeptical that cartilage damage is the cause of my pain, since cartilage damage does not always present with pain.
In March 2025, I was now 1.5 years since the MACI surgery. The envelope of function PT approach had allowed me to return to some cycling and hiking, but pain levels were higher than before. PT exercises that were not painful in 2024 started becoming painful. Walking on flat surfaces is much more painful that it used to be, sometimes even 6/10 pain, which is very difficult to live with. With some reluctance, I decided I need to talk with more orthopedic doctors.
I had x-ray and MRI done. The MRI report contained some new findings:
- the tibial tunnel of the graft is positioned anterior to Blumensaat line
- the ACL graft is bowing
- evidence of fat pad impingement
- my tibia is anteriorly translated on my femur
Opinions from surgeons and PTs
As of August 2025, I am in the process of talking to surgeons and PTs about my situation. Below are my summaries of my interactions so far.
Keith Chan
Upon seeing the MRI and understanding that I’ve already tried managing it conservatively, Keith suggested ACL revision. The thinking is that the anterior graft placement is putting more pressure on my infrapatellar fat pad, which is why it’s so easy for me to trigger painful episodes.
He said my ACL graft is a bit loose based on both the physical exam and the MRI. He also thinks the graft is impinging slightly, which could explain why the ACL has loosened despite me never returning sport since the initial ACLR six years ago.
Keith also said that the MACI surgery I underwent was a “long shot” for treating my pain.
Brian Feeley
Brian wants to gather more information about where the pain is coming from before making any kind of recommendation. He set up a follow-on appointment at the beginning of July for an ultrasound-guided lidocaine injection into my fat pad. The idea is that I will have 1-2 hour window to try doing squats and other movements that cause me pain so that we can know if the pain is coming from inside my knee or outside my knee.
I may also be able to assess if my knee feels like it is giving out. He agreed that my ACL is somewhat loose, but he said that only I can know if it is causing instability.
He said Keith’s theory is plausible, but he also said he’s seen ACL grafts with bone tunnels in similar positions to mine where the patient is pain-free and returned to sport successfully.
Seth Sherman
Similar to Brian, Seth pointed out that while my ACL placement is not ideal, it is “in the zip code” and he has patients who returned to sport with an ACL in this location.
Seth ordered full leg length, weight-bearing x-rays to compare how I am putting weight through my knees and to compare the joint space. Thankfully, he said both look good.
Seth said that cartilage damage and scar tissue are the likely causes of pain in my knee, but that there is no clear intervention he would recommend yet with the information he has. He recommended an exploratory arthroscopy to learn more about the state of my knee, i.e. where cartilage needs to be plugged and how much scar tissue is present in/around the fat pad.
I have become skeptical of cartilage damage as a primary driver of pain in my knee, as it doesn’t track very well with my symptoms. Also, I have extensive cartilage damage in the same area of my good knee, and I am pain-free in that knee.
Seth said that doing the MACI without TTO/TTL does not really make sense. There is no point patching cartilage if the patient is just going to wear the area down again.
Lesley Anderson
Lesley says there are three possible causes of my pain: nerve, chondral, and fat pad. Nerve pain causes a burning sensation, which I do not experience, so that leaves chondral and fat pad.
She is retired, but generally recommends finding a doctor who is a good diagnostician. Brian Feeley seems like such a doctor.
She said my options are injections like PRP or cortisone shots, or surgery. She said the goal of the surgery would be to carefully clear up scar tissue in the fat pad. Surgeons differ widely in their ability to do that well (she said Dr. Steadman was really good at this but he passed away).
Her advice pairs nicely with Brian Feeley’s plan.
Just like Seth Sherman, Lesley also said that doing the MACI without TTO/TTL was a strange choice. She said she would only do that in young patients who had acute patellar cartilage trauma, i.e. a divet of cartilage gets damaged from a fall. In older patients where the cartilage damaged is caused by wear-and-tear, there is no point patching cartilage if the patient is just going to wear the area down again.
(Aside: It’s fair to say at this point that Brian Gilmer’s choice of MACI for medial patellar cartilage damage was incorrect. The area was not a pain driver in my knee, so it was the wrong diagnosis, and even if it was correct, it didn’t make sense to do it without TTO/TTL to correct the maltracking that naturally leads to the medial patellar cartilage wear.)
Ed Shin
Ed was focused on the cartilage damage in my knee and the MRI signal showing sub-chondral bone swelling in my patella and tibia. He said to consider an injection to see if I can bring down the inflammation in my knee. He said to be wary of cortisone injections with the presence of MACI cartilage in the knee, so he recommended that I try hyaluronic acid first.
Ed said the ACL felt fine upon physical exam.
Given that other doctors have emphasized the fat pad as the more likely pain source, I asked him if the cause of my pain could be fat pad pain, and he said it was possible. He said patellofemoral pain and fat pain pain can occur together, and that the onset of one can lead to the other. This reminded me of my appointments with Lesley Anderson and Brian Feeley who both stressed the importance of finding the right diagnosis. If I don’t treat the root cause of my pain and inflammation, I may end up treating a symptom.
Claire Robertson
Claire said I definitely have both patellofemoral pain and fat pad pain.
She encouraged me to focus on safe ranges where I can do clean work that do not trigger patellofemoral or fat pad pain. She described the compressive forces in the patella and encouraged me to try to pursue clean exercises between 30 and 60 degrees, which should avoid fat pad pain and the worst patellofemoral pain.
She described many techniques I currently use or have used in the past: BFR, KT tape, NMES/EMS.
She also mentioned trying a Bioskin medializing patellar brace.
She said to try the brace + EMS + limited range exercises for 6 weeks, and, if I don’t make progress, that I am actually a good candidate for an intra-articular cortisone shot to bring down inflammation and get a window in which I can build quad strength.
It’s already been six weeks, so I can share the results. While the brace + EMS did help a little with pain while walking, it and the limited range queue didn’t help much, so I did not make any progress with her suggestions, which led me to pursue a cortisone shot, which I describe below.
Lidocaine injection
In July I had the lidocaine injection that Dr. Feeley ordered. The injection confirmed that the pain is coming from inside my knee joint, not outside. For a few hours, I experienced very little pain. It was glorious.
I did a squat and it was pain-free. I did some agility movements and I could feel the fat pad pain still when pushing off from my right leg. I tested my ACL stability with some basic pivoting and it felt stable to me.
The doctor who performed the injection said it was a useful diagnostic result. I agree - it’s clear that the bulk of my pain is patellofemoral. There is some fat pad pain as well, but the pain stopping me from progressing is patellofemoral.
Cortisone => toradol injection
I also asked this same doctor about doing the intra-articular cortisone shot that Claire recommended. The doctor was hesitant to perform the cortisone shot given the state of my patellar cartilage and the effect cortisone shots can have on cartilage, so we did a toradol injection instead. She said results vary widely from just a few days of pain relief to a few months. For me, sadly, it only provided a few days of reduced pain.
Danny Keller
At the end of July, I spoke to Danny Keller, a PT who works closely with Dr. Feeley at UCSF.
He’s seen patients with patellar cartilage defects before and he said he was quite confident that I have strong patellofemoral pain, and that the pain is caused by the large cartilage defect in the patellar cartilage. Since my MACI graft has delaminated (i.e. failed), we know the defect is now even larger than it was pre-surgery, since the surgeon has to cut out more cartilage to make room for a piece of MACI graft.
He had a different take on the appropriate PT exercises that I should perform, relative to other PTs I have seen. He said to try open chain isometric exercises. The knee extension machine can be rough on the joint, so he said to use thick bands instead.
Generally I have heard to avoid open chain and do only closed chain exercises as I try to build strength, but he said it’s clear I’m not making progress with even simple closed chain exercises, and that open chain isometrics are even safer. I think this is because it’s easier to isolate muscles, and isometrics do not produce shearing forces in the knee like full-range open chain exercises. Just when I think I’ve learned everything, I learn something new!
He also said to only perform these exercises. Rather than perform a long list of exercises, he is trying to only do safe exercises that fatigue the quad, and to perform them multiple times a day.
Interestingly I have actually been able to fatigue the quad with these exercises, so maybe I am finally onto something. I think I’ll know in the next couple weeks if it’s having a positive effect.
The good news is that Danny and Brian Feeley run a clinic together, so they are my care team regardless of if I keep trying to resolve the pain conservatively or if I pursue surgery. I can even setup appointment to see both of them at the same time. For the first time, I feel like I have an excellent, multidisciplinary care team that I can see for the coming years. I’m glad I took the time to get established at UCSF, even if it took about 5 months to get fully established.
6 years of pain and counting
It’s now been over 6 years since the initial ACL surgery and subsequent complications. I cannot express in words how difficult this has been. The best case scenario is that I partially restore normal function in the coming years. By then, I’ll have spent a full decade of my life on this. I will be dealing with this in one form or another for the rest of my life.